Facts About Epilepsy
- 65 million people around the world have epilepsy.
- 3.4 million people (including 470,000 children and 1 million older adults ages 55+) in the United States have epilepsy.
- 35,000 people on Long Island live with epilepsy.
- 1 in 26 people in the United States will develop epilepsy in their lifetime.
- 150,000 people are diagnosed with epilepsy in the United States each year.
- About 1 out of 3 people with epilepsy live with uncontrolled seizures because no available treatment works for them.
- For 6 out of 10 people with epilepsy, the cause of epilepsy is unknown.

Definition of Epilepsy
Epilepsy is a neurological condition, which means it affects the brain, the main part of the nervous system. Epilepsy may also be called a “seizure disorder.” People are usually diagnosed with epilepsy if:
- They have had 2 or more unprovoked seizures.
- They are likely to have more seizures.
- The seizure wasn’t provoked or caused by another treatable medical condition like an infection or diabetes.
Seizures seen in epilepsy are temporary changes in behavior caused by problems with the electrical and chemical activity of the brain. A seizure occurs when there is a temporary change in the way the brain sends electrical signals. When a seizure happens, there is a “short circuit” in the way messages are sent between brain cells. Seizures may look and feel different from one person to the next. What happens during a seizure depends on the area of brain affected.
Epileptic seizures may be caused by:
- Brain injury at birth
- Brain lesions
- Brain infections
- Brain trauma
- Changes in brain development
- Stroke
- Genetics
- Most of the time, however, the cause is unknown.
Epileptic seizures can result in a change in:
- Movement
- Sensation
- Behavior
- Speech
- Awareness
For more information, go to https://www.epilepsy.com/what-is-epilepsy
Seizure Types
GENERALIZED TONIC–CLONIC SEIZURES (previously called GRAND MAL) – characterized by loss of consciousness, falling, convulsions, muscle rigidity, jerking, vomiting, and loss of bladder control. These seizures generally last one to five minutes followed by periods of confusion, headaches, or the need to rest/sleep.
GENERALIZED ABSENCE SEIZURES (previously called PETIT MAL) – characterized by blank staring, rapid blinking, chewing motions. These seizures only last five to ten seconds but can happen often during one day. The person is unaware of what has happened during the seizure.
FOCAL SEIZURES – WITH ALTERED AWARENESS (previously called COMPLEX PARTIAL)- characterized by staring, chewing movements, picking at clothing, random, robotic body movement and wandering, impaired consciousness, being out of touch with surroundings and an inability to respond to questions or commands. These seizures usually last between one and three minutes followed by a period of confusion, unawareness, and the need to rest/sleep.
FOCAL SEIZURE – NO CHANGE IN AWARENESS (previously called SIMPLE PARTIAL SEIZURES) –characterized by jerking of one or more parts of the body, arms, legs, or face, seeing or hearing things that aren’t there, feeling scared, sad, angry, or happy for no reason. These seizures generally last a few seconds to a few minutes. These are the only seizures where the person is fully aware and knows what is happening.
ATONIC SEIZURES (previously called DROP ATTACKS) – characterized by sudden collapse and brief loss of consciousness. These seizures generally last 10-60 seconds, after which they become fully aware and conscious.
MYOCLONIC SEIZURES – characterized by sudden, brief, massive jerks involving all or part of the body, spilling or dropping things. These seizures usually last a few seconds with complete return to awareness.
INFANTILE SPASMS – characterized by sudden body movements, if sitting up, head and arms falling forward, if lying down, knees folding up and arms and head lifting up. These seizures happen in babies, typically between 3 and 24 months old.
FEBRILE SEIZURES – these seizures are not generally considered to be epileptic. Children aged 3 months to 5 or 6 years old may have tonic-clonic seizures when they have a high fever. Febrile seizures occur in 2% to 5% of all children. There is a slight tendency for them to run in families. The vast majority of children with febrile seizures do not have seizures without fever after age 5.
For more information, go to https://www.epilepsy.com/what-is-epilepsy/seizure-types
Epilepsy Syndrome
- Myoclonic epilepsy in infancy
- Genetic epilepsy with febrile seizures plus
- Early infantile DEE (previously called Ohtahara syndrome, early myoclonic encephalopathy)
- Epilepsy of infancy with migrating focal seizures
- Infantile epileptic spasms syndrome (previously called Infantile Spasms or West syndrome)
- Dravet syndrome (previously called severe myoclonic epilepsy in infancy)
- Childhood occipital visual epilepsy (previously called Gastaut syndrome or late-onset benign occipital epilepsy)
- Photosensitive occipital lobe epilepsy
- Childhood absence epilepsy
- Epilepsy with myoclonic absences
- Epilepsy with eyelid myoclonia (previously called Jeavons syndrome)
- Epilepsy with myoclonic-atonic seizures (previously called myoclonic atonic epilepsy or Doose syndrome)
- Lennox-Gastaut syndrome
- Developmental/epileptic encephalopathy with spike wave activation in sleep (previously called continuous spike-wave in sleep, electrical status epilepticus in sleep or Landau-Kleffner syndrome)
- Febrile infection-related epilepsy syndrome (FIRES)
- Hemiconvulsion-hemiplegia-epilepsy
- Mesial temporal lobe epilepsy with hippocampal sclerosis
- Familial temporal lobe epilepsy
- Sleep-related hypermotor epilepsy
- Familial focal epilepsy with variable foci
- Epilepsy with auditory features
- Epilepsy with reading induced seizures
- Juvenile absence epilepsy
- Juvenile myoclonic epilepsy
- Epilepsy with generalized tonic-clonic seizures alone
- Rasmussen syndrome Progressive myoclonus epilepsies
For more information, go to https://www.epilepsy.com/what-is-epilepsy/syndromes
Psychogenic Non-Epileptic Seizures or Events (PNES/PNEE)
- PNES are attacks that may look like epileptic seizures but are not epileptic and instead are caused by psychological factors.
- Sometimes a specific traumatic event can be identified.
- PNES are sometimes referred to as psychogenic events, psychological events, or nonepileptic seizures (NES).
- The only reliable test to positively make the diagnosis of PNES is video EEG monitoring.
- Treatment with cognitive behavior therapy and serotonin re-uptake inhibitors has been shown to be effective.
- More research is needed to find additional ways to treat PNES.
For more information, go to https://www.epilepsy.com/stories/truth-about-psychogenic-nonepileptic-seizures
Treatment for Epilepsy
The majority of epileptic seizures are controlled by medication, particularly anti-epileptic drugs. The type of treatment prescribed will depend on several factors, including the frequency and severity of the seizures and the person’s age, overall health, and medical history.
- Anti-seizure medications control seizures in 2 out of 3 people
- Implanted stimulation devices such as Vagal Nerve Stimulation and Responsive Neuro-Stimulation
- Medically prescribed dietary therapy such as the Ketogenic Diet; Modified Atkins Diet; Low Glycemic Index Diet
- Epilepsy Surgery
Evaluation by an epilepsy specialist (epileptologist) is critical when medicines are NOT working!
For more information, go to https://www.epilepsy.com/treatment
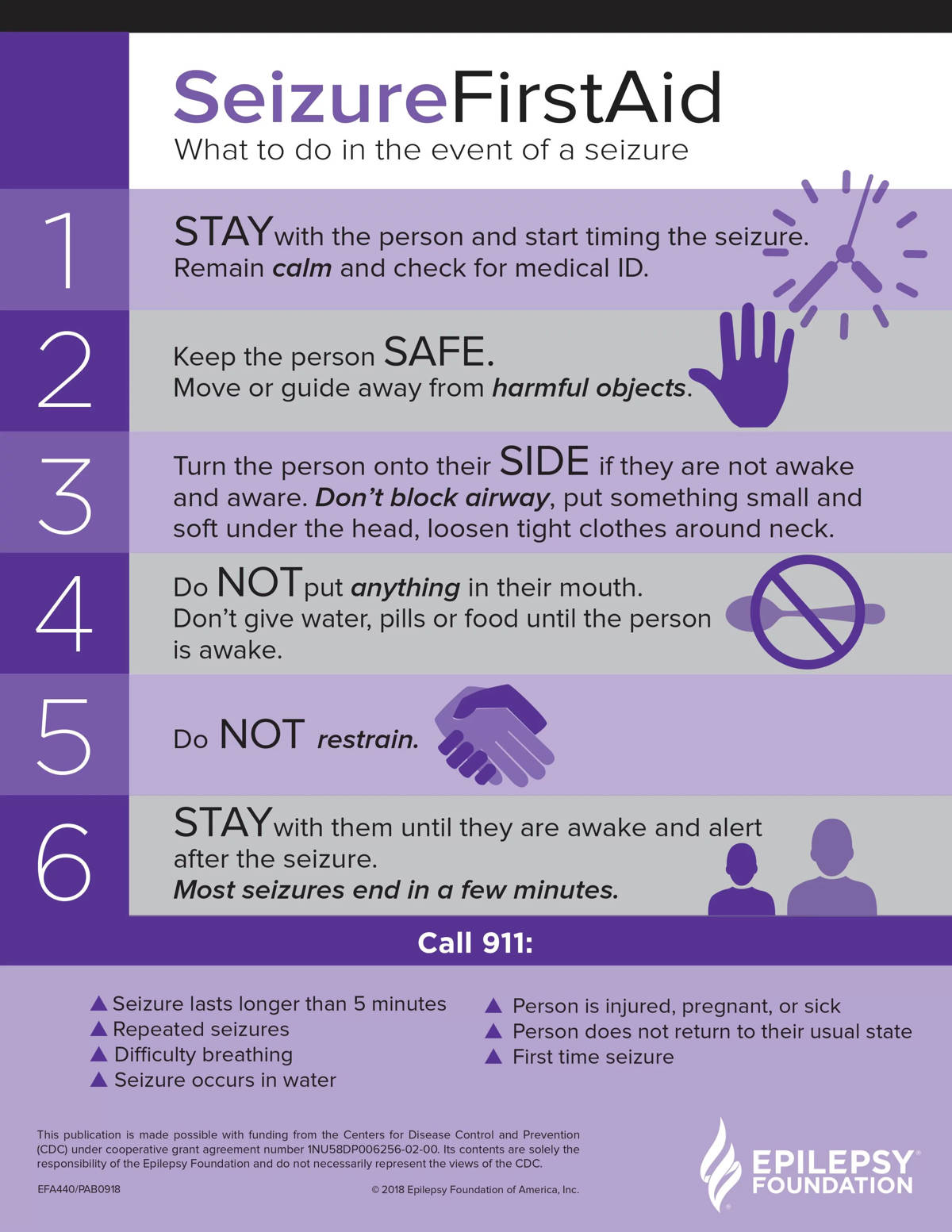
First Aid for Seizures
 The majority of epileptic seizures are controlled by medication, particularly anti-epileptic drugs. The type of treatment prescribed will depend on several factors, including the frequency and severity of the seizures and the person’s age, overall health, and medical history.
The majority of epileptic seizures are controlled by medication, particularly anti-epileptic drugs. The type of treatment prescribed will depend on several factors, including the frequency and severity of the seizures and the person’s age, overall health, and medical history.
- Anti-seizure medications control seizures in 2 out of 3 people
- Implanted stimulation devices such as Vagal Nerve Stimulation and Responsive Neuro-Stimulation
- Medically prescribed dietary therapy such as the Ketogenic Diet; Modified Atkins Diet; Low Glycemic Index Diet
- Epilepsy Surgery
Evaluation by an epilepsy specialist (epileptologist) is critical when medicines are NOT working!
For more information, go to https://www.epilepsy.com/treatment
